Patient Resources
- Osteoporosis
- Osteoporosis Medications
- Covenant Health Osteoporosis Programs
- Osteoporosis and COVID-19
- Other Resources
Osteoporosis
➨ Overview
- Osteoporosis occurs when there is a reduction in the mass in one’s bones. So called “thinning of the bones” increases your chance for bone fracture, particularly the back, hip or wrist. There are many risk factors for developing osteoporosis, some of which can be prevented. For those with osteoporosis, there are treatment options available which can reduce your chance for fracture.
➨ Frequently Asked Questions
➨ What is osteoporosis?
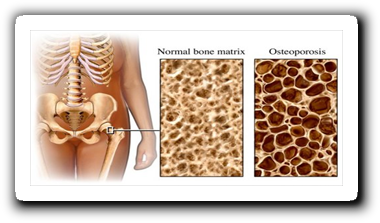
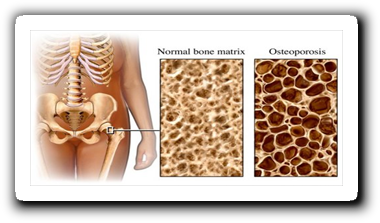
- Bone consists of two key components called hydroxyapatite and osteoid. In osteoporosis, there is a reduction of both of these components of bone.
➨ Are osteoporosis and osteoarthritis the same thing?
- While they sound similar, they are in fact very different conditions. Osteoarthritis is a problem with joints which can cause pain and functional disability. Osteoporosis is bone thinning. Unless you break a bone, it does not directly cause pain or disability. Click here for more information on osteoarthritis.
➨ Why does osteoporosis happen?
- Bone formation is regulated by two cell types, one causes bone formation (osteoblasts) and one causes bone breakdown (osteoclasts). In normal healthy bone, these cells work together, slowly breaking down older bone and replacing it with new bone over long periods of time. In osteoporosis, bone breakdown occurs faster than bone formation, reducing the overall bone mass.
➨ Why is having thinner bones a problem?
- Patients with osteoporosis have an increased risk for breaking their bones. Further, these fractures can happen with minimal trauma. The most common fractures seen in osteoporosis are fractures of the hip, vertebrae and wrist.
➨ How common is osteoporosis?
- Osteoporosis is very common. Some studies estimate 50% of people over the age of 55 may have osteoporosis and many more at risk for developing osteoporosis. The majority are women.
➨ What are risk factors for developing osteoporosis?
- There are many factors which may increase your risk for developing osteoporosis. Some of these cannot be prevented. They include:
- Increasing age
- Female gender
- Early Menopause
- A family history of an osteoporotic fracture
- A previous fracture thought to be due to osteoporosis
- Certain diseases, including but not limited to rheumatoid arthritis, hyperparathyroidism, and hyperthyroidism
- Many other risk factors can be reduced, including:
- Smoking
- Excessive Alcohol Use
- Excessive Caffeine Intake
- Low Weight
- Poor Calcium Intake
- Certain medications, including glucocorticoids (steroids).
➨ How do I know if I have osteoporosis? Does it hurt?
- Most people who have osteoporosis do not know it unless they get tested.
- Unless you have had a fracture, it should not cause pain.
- Some people with osteoporosis may notice loss of weight, or more of a stoop in their back, which can be due to undiagnosed verterbral fractures.
➨ What is the test for osteoporosis?
- Osteoporosis is best tested for using a machine called a DEXA scan. It is a very low radiation safe test which measures the bone density of the lower back and hip.
➨ If I am diagnosed with osteoporosis, what is my risk of breaking a bone?
- The risk of fracture depends on many different things. While your bone density as measured by the DEXA scan is an important component to determine your risk, it is also important to consider your age, previous fractures, other medical conditions and medications. It is important your doctor has all this information to help determine your risk.
- With the appropriate information, you and your physician can estimate your risk of breaking a bone over the next 10 years as either low (<10%), medium (10-20%) or high (>20%).
➨ My doctor told me I have osteopenia. Is that the same as osteoporosis? Does this need treatment?
- Osteopenia is a term that has been used for patients who demonstrate low bone mass on DEXA scan, but not low enough to be called osteoporosis.
- Treatment may or may not be recommended, depending on your age and other risk factors you may have for a fracture.
➨ I have been told I should consider treatment for osteoporosis.
- There are many medication options available for osteoporosis, with a class of medications called bisphosphonates being the most common. Discuss with your physician which is right for you.
- There are also some very important steps which you can take which are not prescribed by your physician. They include:
- Dietary changes (click here for some ideas)
- Daily calcium intake: 500mg three times per day
- Daily Vitamin D intake: 800-2000 Units per day
- Regular weight bearing exercise (E.g. walking)
➨ I do not have osteoporosis, but I have been started on glucocorticoids (steroids/prednisone).
- Glucocorticoids can cause a significant loss of bone mass, particularly for those using them for at least 3-6 months. Patients who require glucocorticoids for at least this long should discuss with their physicians whether or not preventative treatment for developing osteoporosis is right for them.
➨ What can I do to reduce my chance of developing osteoporosis?
- There are many things we can all do to improve our bone health. They include:
- Meet daily calcium needs from diet and/or supplement if needed. Adults >50 require 1200mg per day. Adults 50 and under require: 1000mg per day.
- Take vitamin D supplement daily. Most adults over 50 or those younger adults at high risk of osteoporosis should take 800 – 2,000 IU daily.
- Regular weight bearing exercise.
- For some tips on foods that may help, click here.
➨ What else is important to know about osteoporosis?
- Remember: The ultimate goal of treating osteoporosis is not necessarily making the bones strong again. The goal is to safely lower your risk of breaking a bone.

Covenant Health Osteoporosis Programs


➨ Welcome to the Covenant Health Osteoporosis program information page.
- Osteoporosis is a skeletal (bone) disorder characterized by low bone mass. The bones become more porous and fragile putting them at greater risk of fracture. One in four women and one in eight men will develop low bone density. Osteoporosis can be managed with medical and pharmacological treatment, appropriate exercise, and nutrition and lifestyle changes. (Osteoporosis Canada)
➨ Program Information
- The goals of this program are to gain a better understanding of osteoporosis, improve posture and strength, prevent falls and minimize the risk of sustaining a fracture. You will receive practical information, exercise advice and tips on how to perform daily activities safely. The programs from Covenant Health are offered through the Misericordia Community Hospital and Grey Nuns Community Hospital, using different formats. This allows you to select the approach that works for you and your lifestyle.You do not require a doctor’s referral to attend the program, however, you do need a medical diagnosis of osteoporosis from your doctor. A recent bone mineral density scan is helpful, preferably done within the last 12 months.
These programs are offered at no cost to participants.
➨ Osteoporosis Program at the Grey Nuns Community Hospital
- In person assessment and treatment
- Participants are seen by a Physical Therapist
- Allows for individualized instruction and education, tailored to your specific needs
- Suitable for patients in Edmonton and surrounding area
- Grey Nuns Virtual Exercise Class
- Follow up class to the Grey Nuns Physiotherapy sessions and Misericordia virtual class. Weekly virtual exercise class run by a therapy assistant, runs for 8 weeks
- For Alberta residents
- Requires suitable technology to participate
To print this information for the Grey Nuns, please click here.
For more information on the programs at the Grey Nuns, click on this link:
https://covenanthealth.ca/locations/grey-nuns-community-hospital/osteoporosis-program
➨ Osteoporosis Program at the Misericordia Community Hospital
- Virtual program led by a Physical Therapist, also includes sessions with Dietitian and Pharmacist. Program includes education as well as activities (exercise, balance activities)
- Runs weekly for 7 weeks
- For Alberta Residents
- Requires suitable technology to participate
- Upon completion of this program, participants can join the Grey Nuns Virtual Exercise class
To print this information for the Misericordia, please click here.
For more information on the programs at the Misericordia, click on this link:
https://covenanthealth.ca/locations/misericordia-community-hospital/osteoporosis-program
For general information on Covenant Osteoporosis programs, click on this link:
https://covenanthealth.ca/services/osteoporosis
Osteoporosis and COVID-19
This is a summary of recommendations from Osteoporosis Canada released on March 23 2021, which are consistent with the recommendations put out by the ASMBR, AACE, Endocrine Society, ECTS, IOF and NOF.
➨ Does osteoporosis increase the risk or severity of COVID-19 infections?
- No there is no evidence of this reported to date.
➨ Should I get the COVID-19 vaccine if I have osteoporosis?
- Yes, having osteoporosis or being on treatment for osteoporosis should not be a reason to not receive the COVID-19 vaccine.
➨ What should I do with my osteoporosis medication if I am going to get my COVID-19 vaccine?
- If you are taking an oral bisphosphonate (alendronate, risedronate), you can continue it without any change in dosing.
- If you are taking teriparatide (Forteo) and have not had injection site reactions, you can continue taking it without any change in dosing.
➨ Because COVID-19 vaccine can give you mild flu like reactions and/or injection site reactions and so can IV zoledronic acid (Aclasta), injection denosumab (Prolia) and injection romosozumab (Evenity), the following is recommended:
- If you are taking IV zoledronic acid (Aclasta), you should separate the IV infusion of zoledronic acid and the COVID-19 vaccine by 1 week.
- If you are taking denosumab (Prolia), you should separate the denosumab injection and the COVID-19 vaccine by 4-7 days.
- If you are taking romosozumab (Evenity), you should separate the romosozumab injection and the COVID-19 vaccine by 4-7 days.
For all injections, it is recommend that you do them at a different site from the COVID-19 vaccine, which is generally injected into you upper arm area.
To read the full Osteoporosis Canada statement, click here: https://osteoporosis.ca/covid-19-vaccination-and-osteoporosis-drug-therapy/
Other Resources
➨ Osteoporosis Canada
A national organization serving people with osteoporosis by providing education, advocacy, and strategic investment into osteoporosis research.
Resources of particular mention:
- Calcium Calculator
- Too Fit to Fracture handout
➨ Finding Balance Alberta
Developed and led by the Injury Prevention Centre in Edmonton, Finding Balance is an education program and public awareness campaign to educate and empower older adults to stay independent and prevent falls.
Resources of particular mention:
- Activity Tips and Programming
- Falls Risk Self-Assessment Quiz
- downloadable resources, some of which are available in 13 different languages
- help for caregivers of older adults
➨ Bone Fit
Bone Fit is evidence-informed exercise training for healthcare professionals and exercise practitioners. It was developed by Osteoporosis Canada in conjunction with experts in the area of osteoporosis and exercise to help patients with osteoporosis exercise safely.
Resources of particular mention:
- Locator Map which can be used to find therapists with this specific training
➨ Government of Canada
The Safe Living Guide – A Guide to Home Safety for Seniors
https://www.canada.ca/en/public-health/services/health-promotion/aging-seniors/publications/publications-general-public/safe-living-guide-a-guide-home-safety-seniors.html
➨ Melio Guide
www.melioguide.com/activities-of-daily-living
Based out of Ireland, this resource was created for men and women to intelligently build stronger bones, a stronger body, and reduce fall risk.
Resources of note:
- Activities of Daily Living–tips and videos for specific activities like shoveling snow, mowing the lawn, lifting items in and out of an oven, etc.
➨ National Osteoporosis Foundation
Coming from the United States, this organization is dedicated to preventing osteoporosis and broken bones, promoting strong bones for life, and reducing human suffering through programs of public and clinician awareness, education, advocacy, and research.
Osteoporosis
Osteoporosis
➨ Overview
- Osteoporosis occurs when there is a reduction in the mass in one’s bones. So called “thinning of the bones” increases your chance for bone fracture, particularly the back, hip or wrist. There are many risk factors for developing osteoporosis, some of which can be prevented. For those with osteoporosis, there are treatment options available which can reduce your chance for fracture.
➨ Frequently Asked Questions
➨ What is osteoporosis?
- Bone consists of two key components called hydroxyapatite and osteoid. In osteoporosis, there is a reduction of both of these components of bone.
➨ Are osteoporosis and osteoarthritis the same thing?
- While they sound similar, they are in fact very different conditions. Osteoarthritis is a problem with joints which can cause pain and functional disability. Osteoporosis is bone thinning. Unless you break a bone, it does not directly cause pain or disability. Click here for more information on osteoarthritis.
➨ Why does osteoporosis happen?
- Bone formation is regulated by two cell types, one causes bone formation (osteoblasts) and one causes bone breakdown (osteoclasts). In normal healthy bone, these cells work together, slowly breaking down older bone and replacing it with new bone over long periods of time. In osteoporosis, bone breakdown occurs faster than bone formation, reducing the overall bone mass.
➨ Why is having thinner bones a problem?
- Patients with osteoporosis have an increased risk for breaking their bones. Further, these fractures can happen with minimal trauma. The most common fractures seen in osteoporosis are fractures of the hip, vertebrae and wrist.
➨ How common is osteoporosis?
- Osteoporosis is very common. Some studies estimate 50% of people over the age of 55 may have osteoporosis and many more at risk for developing osteoporosis. The majority are women.
➨ What are risk factors for developing osteoporosis?
- There are many factors which may increase your risk for developing osteoporosis. Some of these cannot be prevented. They include:
- Increasing age
- Female gender
- Early Menopause
- A family history of an osteoporotic fracture
- A previous fracture thought to be due to osteoporosis
- Certain diseases, including but not limited to rheumatoid arthritis, hyperparathyroidism, and hyperthyroidism
- Many other risk factors can be reduced, including:
- Smoking
- Excessive Alcohol Use
- Excessive Caffeine Intake
- Low Weight
- Poor Calcium Intake
- Certain medications, including glucocorticoids (steroids).
➨ How do I know if I have osteoporosis? Does it hurt?
- Most people who have osteoporosis do not know it unless they get tested.
- Unless you have had a fracture, it should not cause pain.
- Some people with osteoporosis may notice loss of weight, or more of a stoop in their back, which can be due to undiagnosed verterbral fractures.
➨ What is the test for osteoporosis?
- Osteoporosis is best tested for using a machine called a DEXA scan. It is a very low radiation safe test which measures the bone density of the lower back and hip.
➨ If I am diagnosed with osteoporosis, what is my risk of breaking a bone?
- The risk of fracture depends on many different things. While your bone density as measured by the DEXA scan is an important component to determine your risk, it is also important to consider your age, previous fractures, other medical conditions and medications. It is important your doctor has all this information to help determine your risk.
- With the appropriate information, you and your physician can estimate your risk of breaking a bone over the next 10 years as either low (<10%), medium (10-20%) or high (>20%).
➨ My doctor told me I have osteopenia. Is that the same as osteoporosis? Does this need treatment?
- Osteopenia is a term that has been used for patients who demonstrate low bone mass on DEXA scan, but not low enough to be called osteoporosis.
- Treatment may or may not be recommended, depending on your age and other risk factors you may have for a fracture.
➨ I have been told I should consider treatment for osteoporosis.
- There are many medication options available for osteoporosis, with a class of medications called bisphosphonates being the most common. Discuss with your physician which is right for you.
- There are also some very important steps which you can take which are not prescribed by your physician. They include:
- Dietary changes (click here for some ideas)
- Daily calcium intake: 500mg three times per day
- Daily Vitamin D intake: 800-2000 Units per day
- Regular weight bearing exercise (E.g. walking)
➨ I do not have osteoporosis, but I have been started on glucocorticoids (steroids/prednisone).
- Glucocorticoids can cause a significant loss of bone mass, particularly for those using them for at least 3-6 months. Patients who require glucocorticoids for at least this long should discuss with their physicians whether or not preventative treatment for developing osteoporosis is right for them.
➨ What can I do to reduce my chance of developing osteoporosis?
- There are many things we can all do to improve our bone health. They include:
- Daily calcium intake. Adults over the age of 50 should have meet daily calcium needs from diet and/or supplement if needed. Adults >50 require 1200mg per day. Adults 50 and under require: 1000mg per day.
- Daily VTake vitamin D supplement daily. Most adults over 50 or those younger adults at high risk of osteoporosis should take 800 – 2,000 IU daily.
- Regular weight bearing exercise.
- For some tips on foods that may help, click here.
➨ What else is important to know about osteoporosis?
- Remember: The ultimate goal of treating osteoporosis is not necessarily making the bones strong again. The goal is to safely lower your risk of breaking a bone.

Osteoporosis Medications
Covenant Health Osteoporosis Programs
Covenant Health Osteoporosis Programs


➨ Welcome to the Covenant Health Osteoporosis program information page.
- Osteoporosis is a skeletal (bone) disorder characterized by low bone mass. The bones become more porous and fragile putting them at greater risk of fracture. One in four women and one in eight men will develop low bone density. Osteoporosis can be managed with medical and pharmacological treatment, appropriate exercise, and nutrition and lifestyle changes. (Osteoporosis Canada)
➨ Program Information
- The goals of this program are to gain a better understanding of osteoporosis, improve posture and strength, prevent falls and minimize the risk of sustaining a fracture. You will receive practical information, exercise advice and tips on how to perform daily activities safely.
The programs from Covenant Health are offered through the Misericordia Community Hospital and Grey Nuns Community Hospital, using different formats. This allows you to select the approach that works for you and your lifestyle.
You do not require a doctor’s referral to attend the program, however, you do need a medical diagnosis of osteoporosis from your doctor. A recent bone mineral density scan is helpful, preferably done within the last 12 months.
These programs are offered at no cost to participants.
➨ Osteoporosis Program at the Grey Nuns Community Hospital
- In person assessment and treatment
- Participants are seen by a Physical Therapist
- Allows for individualized instruction and education, tailored to your specific needs
- Suitable for patients in Edmonton and surrounding area
- Grey Nuns Virtual Exercise Class
- Follow up class to the Grey Nuns Physiotherapy sessions and Misericordia virtual class. Weekly virtual exercise class run by a therapy assistant, runs for 8 weeks
- For Alberta residents
- Requires suitable technology to participate
To print this information for the Grey Nuns, please click here.
For more information on the programs at the Grey Nuns, click on this link:
https://covenanthealth.ca/locations/grey-nuns-community-hospital/osteoporosis-program
➨ Osteoporosis Program at the Misericordia Community Hospital
- Virtual program led by a Physical Therapist, also includes sessions with Dietitian and Pharmacist. Program includes education as well as activities (exercise, balance activities)
- Runs weekly for 7 weeks
- For Alberta Residents
- Requires suitable technology to participate
- Upon completion of this program, participants can join the Grey Nuns Virtual Exercise class
To print this information for the Misericordia, please click here.
For more information on the programs at the Misericordia, click on this link:
https://covenanthealth.ca/locations/misericordia-community-hospital/osteoporosis-program
For general information on Covenant Osteoporosis programs, click on this link:
https://covenanthealth.ca/services/osteoporosis
Osteoporosis and COVID-19
Osteoporosis and COVID-19
This is a summary of recommendations from Osteoporosis Canada released on March 23 2021, which are consistent with the recommendations put out by the ASMBR, AACE, Endocrine Society, ECTS, IOF and NOF.
➨ Does osteoporosis increase the risk or severity of COVID-19 infections?
- No there is no evidence of this reported to date.
➨ Should I get the COVID-19 vaccine if I have osteoporosis?
- Yes, having osteoporosis or being on treatment for osteoporosis should not be a reason to not receive the COVID-19 vaccine.
➨ What should I do with my osteoporosis medication if I am going to get my COVID-19 vaccine?
- If you are taking an oral bisphosphonate (alendronate, risedronate), you can continue it without any change in dosing.
- If you are taking teriparatide (Forteo) and have not had injection site reactions, you can continue taking it without any change in dosing.
➨ Because COVID-19 vaccine can give you mild flu like reactions and/or injection site reactions and so can IV zoledronic acid (Aclasta), injection denosumab (Prolia) and injection romosozumab (Evenity), the following is recommended:
- If you are taking IV zoledronic acid (Aclasta), you should separate the IV infusion of zoledronic acid and the COVID-19 vaccine by 1 week.
- If you are taking denosumab (Prolia), you should separate the denosumab injection and the COVID-19 vaccine by 4-7 days.
- If you are taking romosozumab (Evenity), you should separate the romosozumab injection and the COVID-19 vaccine by 4-7 days.
For all injections, it is recommend that you do them at a different site from the COVID-19 vaccine, which is generally injected into you upper arm area.
To read the full Osteoporosis Canada statement, click here: https://osteoporosis.ca/covid-19-vaccination-and-osteoporosis-drug-therapy/
Other Resources
Other Resources
➨ Osteoporosis Canada
A national organization serving people with osteoporosis by providing education, advocacy, and strategic investment into osteoporosis research.
Resources of particular mention:
- Calcium Calculator
- Too Fit to Fracture handout
➨ Finding Balance Alberta
Developed and led by the Injury Prevention Centre in Edmonton, Finding Balance is an education program and public awareness campaign to educate and empower older adults to stay independent and prevent falls.
Resources of particular mention:
- Activity Tips and Programming
- Falls Risk Self-Assessment Quiz
- downloadable resources, some of which are available in 13 different languages
- help for caregivers of older adults
➨ Bone Fit
Bone Fit is evidence-informed exercise training for healthcare professionals and exercise practitioners. It was developed by Osteoporosis Canada in conjunction with experts in the area of osteoporosis and exercise to help patients with osteoporosis exercise safely.
Resources of particular mention:
- Locator Map which can be used to find therapists with this specific training
➨ Government of Canada
The Safe Living Guide – A Guide to Home Safety for Seniors
https://www.canada.ca/en/public-health/services/health-promotion/aging-seniors/publications/publications-general-public/safe-living-guide-a-guide-home-safety-seniors.html
➨ Melio Guide
www.melioguide.com/activities-of-daily-living
Based out of Ireland, this resource was created for men and women to intelligently build stronger bones, a stronger body, and reduce fall risk.
Resources of note:
- Activities of Daily Living–tips and videos for specific activities like shoveling snow, mowing the lawn, lifting items in and out of an oven, etc.
➨ National Osteoporosis Foundation
Coming from the United States, this organization is dedicated to preventing osteoporosis and broken bones, promoting strong bones for life, and reducing human suffering through programs of public and clinician awareness, education, advocacy, and research.
